Founded in 1947, the Division of Gastroenterology and Hepatology has had a long history of excellence that continues today.
With 80 faculty, 25 fellows, and over 150 staff, we are one of the largest gastroenterology practices in the country and a leader in the prevention, diagnosis, and treatment of all diseases of the gastrointestinal system, from simple to complex, including those of the esophagus, stomach, small intestine, colon, rectum, liver, gallbladder, pancreas, and biliary tract.
Patient Care
We have established a number of clinical centers of excellence:
- Esophageal Disorders Program
- Functional Bowel Disorders Program
- Hepatology Program
- Inflammatory Bowel Disease (IBD) Program
- Interventional Endoscopy Program
- Michigan Bowel Control Program
- Wilson Disease Program
Research
In addition to being leaders in the clinic, our faculty are also leaders in their respective areas of research, which span such varied interests as the role of peptides in the brain–gut interactions in functional bowel diseases to innovative treatments of viral hepatitis and liver cancer. Learn more.
Education and Training
The Division of Gastroenterology and Hepatology offers three unique fellowship programs:
- 3-year Gastroenterology Fellowship Training Program that includes a NIH-funded T32 Clinical Research Training Program track
- Advanced Endoscopy Fellowship Program (4th year)
- Transplant Hepatology Fellowship Program (4th year)
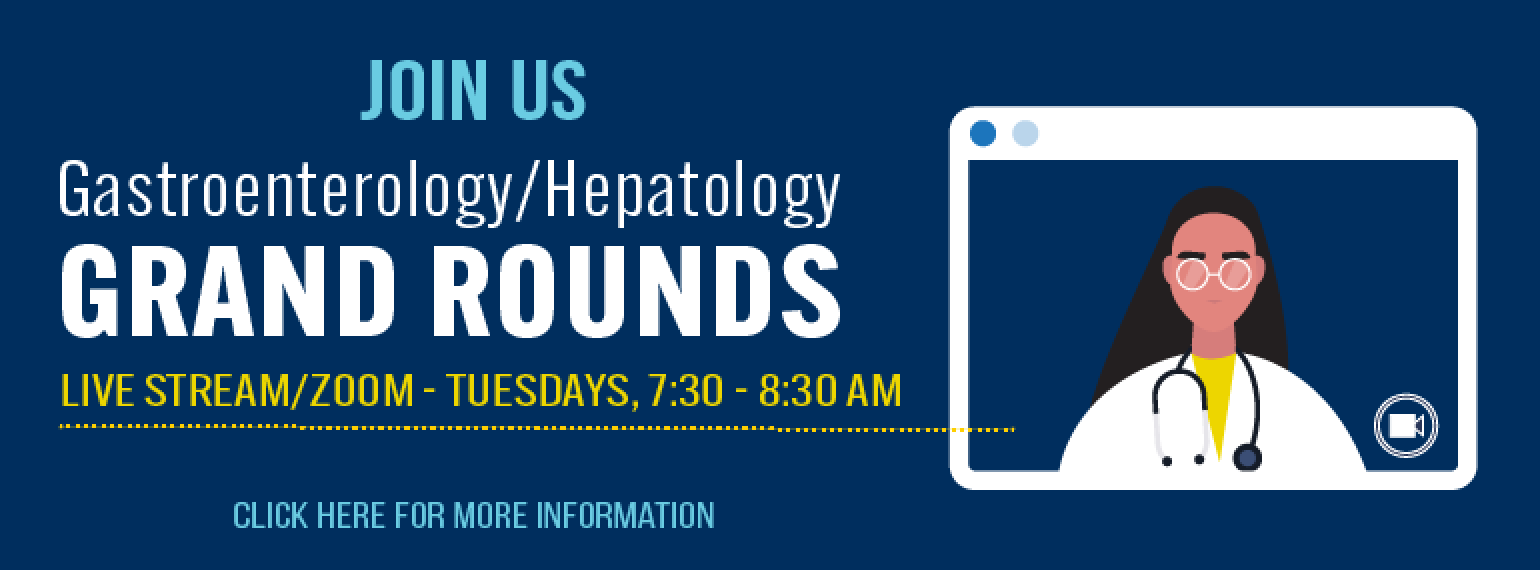
We also participate in other training within the Department of Internal Medicine and the University of Michigan Medical School. In addition, we have numerous education programs that are provided to physicians and patients of southeastern Michigan. Our Continuing Medical Education network offers three multi-day courses and over 100 single lectures annually. Learn more.
Diversity, Equity, Inclusion, and Well-Being
The Department of Internal Medicine (DOIM) Division of Gastroenterology and Hepatology is committed to creating and cultivating a diverse and inclusive community that provides our faculty, learners, and staff with the opportunities and support they need to thrive. Visit the DOIM Office of Diversity, Equity, Inclusion, and Well-Being to learn more.